Picture this: a mid-season footballer plants her foot, twists sharply, and for a moment the pain just “feels like a sprain.” But underneath that familiar phrase lies a hidden hazard: the dreaded high ankle sprain, a discrete but dangerous injury to the distal tibio-fibular “syndesmosis.”
Left undetected or treated too casually, it can haunt your recovery, sideline you far longer than expected, and even sow the seeds of chronic ankle instability. At Destiny Health we’ve seen the confusion, the delayed diagnoses, and the frustration.
Let’s dive into what a syndesmosis injury is, how to spot it (and how it’s missed), and, crucially, how to guide rehabilitation to get back stronger.
Basic Anatomy: the “hidden joint” of the ankle
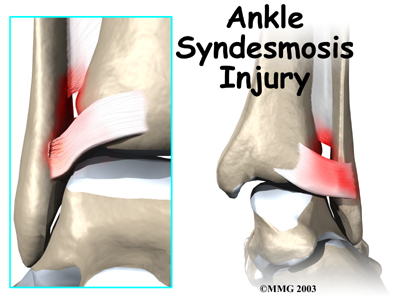
The ankle is not simply the talus perched between tibia and fibula, it’s also stabilised by the syndesmosis joint, which connects the distal ends of the tibia and fibula just above the ankle mortise. Orthobullets+2Physiopedia+2
Key components include:
-
The anterior-inferior tibiofibular ligament (AITFL): runs from the anterolateral tubercle of the tibia to the fibula. Orthobullets+1
-
The posterior-inferior tibiofibular ligament (PITFL): posterior tubercle of the tibia to the lateral malleolus; the strongest syndesmosis component. Orthobullets
-
The interosseous membrane and the interosseous ligament (IOL): which link the tibia and fibula along their shafts and resist separation. Physiopedia
Functionally, the syndesmosis maintains stability of the ankle mortise during talar motion, especially under dorsiflexion and external rotation forces. International Journal of Sports Therapy+1
Common Patterns of Injury

A syndesmosis injury (commonly described as a “high ankle sprain”) typically occurs when the ankle is forced into external rotation (foot turns outward relative to leg) and often with dorsiflexion or a planted foot. Orthobullets
Mechanisms and patterns include:
-
An athlete cuts/pivots, foot fixed and tibia rotates over it → talus drives fibula laterally vs tibia leading to syndesmosis disruption. South Shore Orthopedics+1
-
Less commonly, a direct blow or forced eversion may damage the syndesmosis.
-
Often associated with other injuries: fractures (fibula, medial malleolus, posterior malleolus), deltoid ligament tears, or peroneal tendon injuries. Orthobullets+1
-
Unlike a lateral ligament sprain (ATFL, CFL) which is common, syndesmosis injuries are less frequent but more severe: reported at about 0.5% of all ankle sprains without fracture. Orthobullets
Because of their location and mechanism, high ankle sprains take longer to heal than typical ankle sprains. pmc.ncbi.nlm.nih.gov+1

Clinical Tests Physios Use to Diagnose Them
Detecting a syndesmosis injury requires vigilance: some useful clinical tests and signs include:
-
Squeeze test: compress the tibia and fibula together at mid-calf; reproduction of pain at syndesmosis region suggests injury. Orthobullets+1
-
External rotation test (Kleiger’s test): with foot planted, externally rotate the foot; pain in syndesmosis region is a red flag.
-
Palpation: tenderness just above the ankle joint between tibia and fibula (anterolateral region) and possibly along the interosseous membrane. PubMed
-
Weight-bearing and hop tests (later): In rehab phase, inability to hop or bear weight without pain suggests incomplete resolution. pmc.ncbi.nlm.nih.gov+1
-
Radiographic stress tests / CT / MRI: If there is concern about diastasis (widening) of syndesmosis, imaging is warranted (see below). Orthobullets+1
It’s worth noting that physios must combine findings with mechanism and clinical suspicion, because these injuries are easily missed.
How They Can Be Missed, and Why That Matters
Why do syndesmosis injuries slip through the cracks?
-
Because they often masquerade as “just a sprain” of the ankle. The patient may walk, weight-bear, or feel a lateral ligament pain and the typical “roll ankle” story seems to fit.
-
Swelling may be less dramatic than lateral sprains. One review noted swelling is not always present in syndesmosis injuries. South Shore Orthopedics
-
Standard ankle X-rays may not reveal syndesmotic instability or diastasis clearly. Plain images may appear “normal”. pmc.ncbi.nlm.nih.gov+1
-
Lack of awareness: Because lateral sprains are far more common, clinicians may inadvertently assume the more common injury.
Consequences of missed or delayed diagnosis:
-
Prolonged recovery (weeks to months extra) compared to isolated sprains. pmc.ncbi.nlm.nih.gov+1
-
Persistent pain, instability or recurrent sprains. International Journal of Sports Therapy+1
-
Early arthritis (post-traumatic ankle arthrosis) if the ankle mortise remains incongruent. International Journal of Sports Therapy+1
-
Delayed return to sport or activity, especially in athletes whose ankle stability is critical.
In short: missing the injury isn’t minor, it derails the rehab and outcome.

When is MRI (or Advanced Imaging) Warranted?
Imaging plays a key role beyond the physical exam. General guidance:
-
If the clinical suspicion is high (mechanism, pain, positive physical tests) and the plain radiographs (including mortise view, stress views) are inconclusive (meaning no obvious separation of the tibia and fibula are seen).
-
When you suspect syndesmotic diastasis (gapping), associated fracture, or instability: immediate referral for imaging is indicated. Orthobullets+1 There only needs to be a 1mm gap for future ankle instability to occur.
-
MRI is more sensitive and specific than plain radiographs for assessing syndesmotic ligament integrity, IOL tearing, and associated cartilage/osteochondral lesions. pmc.ncbi.nlm.nih.gov
-
In athletes or high-demand patients whose return to play timeline is critical, imaging early can guide operative vs non-operative decision-making. International Journal of Sports Therapy
Therefore: if you are managing a sprain but the picture is not settling as expected (prolonged pain/instability at 3-4 weeks), consider referral for MRI or specialist imaging.
Rehabilitation Phases: From “ouch” to “game ready”
Once a syndesmosis injury is confirmed or highly suspected, the rehabilitation pathway is more conservative and structured than for a typical lateral ankle sprain. Here’s a three-phase overview:
Phase 1: Acute / Protection (Weeks 0–2/4 depending severity)
-
Goals: reduce pain, swelling; protect the syndesmosis; maintain motion and muscle tone. PubMed+1
-
Strategies: rest/ice/anti-inflammatory as indicated; immobilisation or boot if required; weight-bearing as tolerated but often limited. Sanford Health+1
-
Gentle ROM (avoiding excessive dorsiflexion/rotation) and isometrics for calf/ankle, proximal hip/knee strength. Sanford Health+1
-
Crutches may be required until pain-free gait is restored.
Progression criteria: pain and swelling reduced, ability to tolerate weight-bearing, basic ROM restored.
Phase 2: Subacute / Strength & Control (Weeks approx 3-8)
-
Goals: normalise ROM, restore strength, begin neuromuscular/proprioceptive training. pmc.ncbi.nlm.nih.gov+1
-
Strategies: progress weight-bearing, introduce single-leg stance, wobble board, resisted ankle band exercises, calf raises, hip/knee control. pmc.ncbi.nlm.nih.gov+1
-
Avoid high-impact or cutting/pivoting until control is adequate.
Progress criteria: full painless ROM, strength ~90% of opposite side, successful single-leg balance >30 s, no pain on basic hopping.
Phase 3: Advanced Functional / Return to Sport (Weeks approx 8+ up to 12 or more for athletes)
-
Goals: return to full function or sport-specific activity, prevent re-injury. pmc.ncbi.nlm.nih.gov+1
-
Strategies: agility drills, plyometrics (hops, bounding), sport-specific movement patterns, cutting/pivoting, progression of load and speed. pmc.ncbi.nlm.nih.gov
-
In athletes, the timeline may extend to 3-6 months depending injury severity and treatment (operative vs non-operative) and demands. International Journal of Sports Therapy+1
-
Use of brace/taping on return may be advised in first season back. pmc.ncbi.nlm.nih.gov
Progress criteria: symptom-free activity at full speed, hop test symmetrical, confident cutting/pivoting, sport-specific performance equal to pre-injury.
Closing the Loop: From Threat to Triumph
Remember our footballer? She thought she’d simply “rolled” her ankle. Six weeks later, she’s still limping, back into training but limping sideways, avoiding full cuts, because the syndesmosis injury was missed.
Imagine the frustration, the lost season, the nagging instability. Now imagine instead: immediate suspicion, early imaging, a rehab protocol that respects the unique anatomy, and a purposeful return plan. The difference is huge.
At Destiny Health, we don’t just treat “ankle sprains”. We recognise when a presentation might hide a syndesmosis injury, we advocate for the right diagnostics, and we guide our clients through a rehab roadmap informed by the latest evidence.
Because when the ankle betrays you once, future risk skyrockets. But when you commit to a smart, staged, aggressive-but-safe rehab, you turn the story around. The ankle can become stronger, more resilient, and the fear of “what if I twist it again?” fades.
Action Plan
-
Be suspicious of a high ankle sprain when the mechanism involves external rotation or dorsiflexion with a planted foot.
-
Perform clinical tests: squeeze test, external rotation test, palpation above ankle joint.
-
Refer for imaging (MRI or stress CT) if pain/instability persists, weight-bearing is difficult, or plain films inconclusive.
-
Follow a structured three-phase rehab program (protect → restore → return) with clear progression criteria—avoid rushing.
-
Education is key: it’s not “just a sprain”. Missed time = delayed return + risk of early arthritis. Encourage compliance, balance training, neuromuscular control.
-
Monitor return to activity with hop tests, strength measures, and sport-specific drills. Ensure readiness before full return.
References
Clanton, T. O., & Paul, P. (2002). Syndesmosis injuries in athletes. Foot & Ankle Clinics of North America, 7(3), 529-549.
“Diagnosis and treatment of acute ankle injuries: development of an evidence-based algorithm”. (2012). Orthopaedics Review (Pavia).
“High Ankle Sprain & Syndesmosis Injury”. (2023). Orthobullets. Retrieved from https://www.orthobullets.com/foot-and-ankle/7029/high-ankle-sprain-and-syndesmosis-injury
Porter, D. A. (2012). Optimal management of ankle syndesmosis injuries. Foot & Ankle Clinics of North America.
Rehabilitation of syndesmotic (high) ankle sprains. (2010). Sports Health. 2(6), 461-467.
“Syndesmotic Ankle Sprains”. (n.d.). Physiopedia. Retrieved from https://www.physio-pedia.com/Syndesmotic_Ankle_Sprains
Seybold, J., Grindal, E., & Solie, B. (2021). Syndesmosis repair rehab protocol: TightRope and internal brace. TCO MN.
“Typical Recovery for a High Ankle Sprain”. (2024). Motion Orthopaedics. Retrieved from https://www.motionorthodocs.com/blog/typical-recovery-for-a-high-ankle-sprain/
High Ankle Sprain Rehabilitation Guideline. (n.d.). Sanford Health. Retrieved from https://www.sanfordhealth.org/-/media/org/files/medical-services/physical-therapy/014000-01456-flyer-sosm-high-ankle-sprain-rehab-guideline-8_5x11.pdf
The Prehab Guys. (n.d.). High ankle sprain rehab: sample program. Retrieved from https://theprehabguys.com/high-ankle-sprain/
When you treat an ankle sprain, always ask: is this just a lateral ligament twist, or could the syndesmosis be involved? Catching it early changes everything. At Destiny Health, our mission is simple: turn hidden threats into visible recovery plans. Let’s keep you in the game, not sidelined wondering “what if”.
Had an ankle injury?
Book your FREE ASSESSMENT on our home page today!
You only pay if you agree with the management plan and wish to proceed.

